A simple kitchen mishap or a backyard scrape may result in cuts. Sometimes, they tend to be just minor nicks or even end up as severe lacerations. The question is, how to know if a cut needs stitches? When do you need emergency help for circumstances such as these?
Read more to know about having stitches for cuts and other recovery options to help you go back to your regular routine.
What Are Stitches?
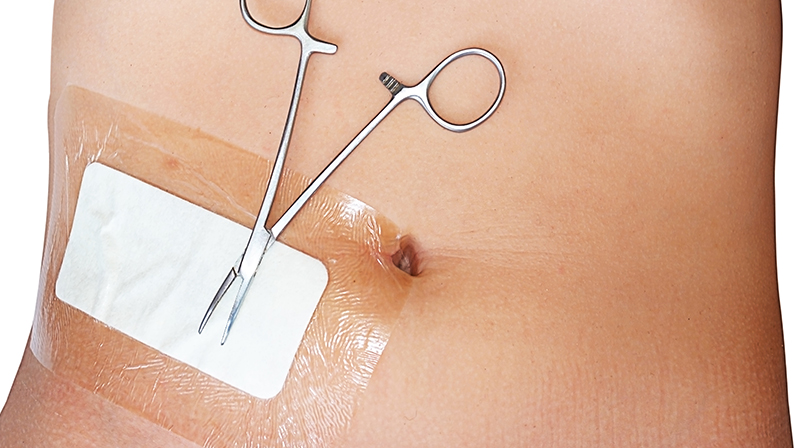
Stitches, also known as sutures, are medical procedures where a healthcare professional sews up a wound or incision to promote healing.
Typically made of materials like silk, nylon, or absorbable substances, stitches hold the wound edges together, preventing infection and allowing the natural healing process to occur.
Stitches are commonly used for deep cuts, surgical incisions, or injuries that require additional support for proper recovery.
Types of Stitches
Sutures come in various types, each tailored to specific wound characteristics:
- Interrupted Stitches: These are individual stitches placed at intervals along the wound, providing flexibility and easy removal.
- Continuous Sutures (Running Stitches): A single, continuous thread secures the wound and is often used for long incisions with minimal tension.
- Subcuticular Stitches: Placed beneath the skin’s surface, these stitches reduce scarring and are ideal for cosmetic procedures or delicate skin areas.
How To Know If A Cut Needs Stitches?
When faced with a cut, determining whether stitches are necessary involves a careful assessment of various factors.
How big is it?
Larger wounds, especially those with gaping edges, may struggle to heal effectively on their own. The size helps gauge the potential requirement for medical intervention.
How badly is it bleeding?
Excessive bleeding can be alarming and may indicate a need for stitches. Assess the severity of bleeding to differentiate between a minor surface cut and a deeper wound that might require professional closure to control bleeding and promote proper healing.
What caused it?
The nature of the injury is a crucial factor in determining if stitches are necessary. Deeper cuts resulting from sharp objects or traumatic incidents may pose a higher risk of infection and may require stitches to facilitate healing and minimize complications.
Where is the wound?
The location of the wound on the body influences the decision-making process. Cuts over joints or areas prone to movement might benefit from stitches to prevent tension and ensure the wound closes neatly, reducing the risk of scarring and complications.
Is it getting infected?
Monitoring the wound for signs of infection is essential. If the cut shows redness, swelling, or pus, it may indicate infection, warranting medical attention.
If you don’t know how to tell how deep a cut is or you are not sure if your wound is already infected, you need to consult a medical expert immediately.
Signs of Infection to Watch For

During the healing phase, wounds may still be exposed to infections.
Keep a watchful eye on the following symptoms to ensure a healthy healing process:
- Redness around the wound can be a preliminary sign of infection, indicating an inflammatory response to bacteria or foreign substances in the cut. If the redness persists or intensifies, it warrants close attention.
- Red streaks spreading out from the wound are concerning and may signify an advancing infection along the lymphatic vessels. Immediate medical attention is essential if you observe such streaks, as they indicate a more serious infection that could potentially spread.
- Increased swelling around the wound is a common sign of infection. While some swelling is normal during the initial stages of healing, a sudden or persistent increase may suggest an underlying problem that requires professional assessment.
- Warmth radiating from the wound site is another indicator of infection. Infections often generate localized heat due to the body’s immune response. If you notice abnormal warmth, it’s advisable to seek medical advice promptly.
- Pain and tenderness beyond the expected discomfort during the early stages of healing may point to infection. Persistent or worsening pain, especially when accompanied by other signs, should prompt a medical evaluation.
- Pus or drainage from the wound is a clear sign of infection. The presence of yellow or green discharge may indicate the presence of bacteria, and addressing this promptly can prevent further complications.
- Fever is a systemic response to infection. If you experience an unexplained increase in body temperature, it may be a sign that the infection has spread, and medical attention is imperative to prevent worsening conditions.
What Cuts Are Most Prone to Infection?
Certain characteristics and circumstances increase the risk of infections.
Explore the following factors to identify cuts that may demand extra attention and precautionary measures:
- Immunocompromised Individuals: Cuts in individuals with weakened immune systems, such as those with chronic illnesses or undergoing certain medical treatments, are more prone to infections. The body’s ability to fight off pathogens is compromised, heightening the risk of bacterial infiltration in even minor wounds.
- Puncture Wounds: Cuts caused by puncture wounds, such as stepping on a sharp object or animal bites, carry a higher risk of infection. The depth and narrow nature of these wounds create an environment conducive to bacterial growth.
- Contaminated Objects: Cuts sustained from contact with contaminated objects or dirty surfaces are at increased risk of infection. Bacteria present on the object can easily enter the wound.
- Lacerations in High-Bacteria Areas: Cuts in areas of the body with naturally higher bacterial populations, such as the mouth, hands, or genital region, are more prone to infection. Additionally, wounds over joints or areas subject to constant movement may face challenges in maintaining cleanliness, requiring special attention.
- Untreated or Improperly Cleaned Wounds: Cuts that haven’t been promptly and properly cleaned are more susceptible to infection. Failing to remove debris or foreign particles from the wound can create an environment conducive to bacterial growth, leading to complications.
- Diabetic Individuals: Individuals with diabetes often experience delayed wound healing, and their cuts are more prone to infection. Monitoring cuts closely and seeking prompt medical attention is crucial for diabetic individuals to prevent complications and ensure effective healing.
Basic First Aid for Cuts
Cuts are a common part of life, and knowing how to administer basic first aid is crucial for prompt and effective wound care.
Follow these simple steps can make a significant difference in the healing process:
- Clean Your Hands: Before touching the wound, wash your hands thoroughly with soap and water to reduce the risk of infection.
- Stop the Bleeding: Apply gentle pressure to the wound with a clean cloth or sterile bandage. Elevate the injured area if possible to help control bleeding.
- Clean the Wound: Rinse the cut gently under cool running water to remove dirt and debris. Avoid using hydrogen peroxide or alcohol, as they can damage tissue.
- Apply an Antiseptic: Use an antiseptic solution or ointment to help prevent infection. Apply a thin layer to the wound using a clean cotton swab or sterile gauze.
- Cover the Wound: Use a sterile bandage or non-stick sterile gauze to cover the wound. This protects it from dirt and bacteria, promoting a clean, healing environment.
- Change Dressings Regularly: If the bandage becomes wet or dirty, change it to maintain a clean and dry environment for the wound.
- Watch for Signs of Infection: Keep a close eye on the wound for any signs of infection, such as increased redness, swelling, or discharge. Seek medical attention if these signs occur.
- Keep the Area Elevated: Elevate the injured area if possible to reduce swelling and promote healing.
- Take Pain Relievers if Necessary: Over-the-counter pain relievers, such as acetaminophen or ibuprofen, can help manage pain and reduce inflammation. Follow dosage instructions.
When to Seek Professional Medical Attention

While many cuts can be effectively treated with basic first aid at home, certain situations warrant prompt medical attention to ensure proper care and prevent complications. Consult medical help to know the cuts that need stitches vs ones that don’t.
Deep or Wide Cuts
If a cut is deep or has wide edges that don’t easily come together, it may require professional closure to promote optimal healing and minimize scarring.
Excessive Bleeding
If the bleeding persists despite applying pressure or if it’s difficult to control, seek medical attention immediately. Excessive bleeding may indicate a more severe injury.
Objects Embedded in the Wound
Cuts caused by objects such as glass or metal that leave fragments in the wound should be addressed by a healthcare professional to ensure proper removal and reduce the risk of infection.
Signs of Infection
If the wound shows signs of infection, such as increased redness, swelling, warmth, or discharge, consult a healthcare professional promptly. Timely intervention can prevent the infection from spreading.
Difficulty Moving a Joint
Cuts near joints or that affect the movement of a joint may require a professional assessment to ensure proper closure and prevent complications in mobility.
Animal Bites or Human Bites
Wounds from animal bites or human bites often require medical attention due to the risk of infection. Prompt care can minimize the chances of complications.
Dirty or Rusty Objects
Cuts caused by dirty or rusty objects carry an increased risk of infection, and a tetanus shot may be necessary. Seek professional advice to assess the need for a tetanus booster.
Persistent Pain or Numbness
If the pain persists or if you experience numbness around the cut, it’s essential to consult a healthcare professional. These symptoms may indicate nerve damage that requires specialized attention.
Wounds in High-Risk Individuals
Individuals with certain health conditions, such as diabetes or compromised immune systems, should seek professional medical attention for even minor cuts to know when do you need stitches and prevent complications.
Uncertainty About Tetanus Immunization
If you are unsure about your tetanus immunization status and the wound is caused by a potentially contaminated object, consult a healthcare professional to determine if a tetanus shot is necessary.
Remember, when in doubt, it’s always better to seek professional medical advice to ensure the appropriate care for your specific situation.
How Stitches Help with Healing
Stitches can facilitate the healing process of wounds by providing structural support and promoting optimal conditions for recovery. This controlled closure reduces the risk of scarring and complications, allowing the body’s healing mechanisms to function more efficiently.
Visit SilverLake ER for Emergency Stitches Due to a Cut
While minor cuts can often be managed with basic first aid, certain situations demand the expertise of healthcare professionals.
If you find yourself in need of emergency stitches on your finger or you are wondering how to get stitches, don’t hesitate to seek immediate assistance.
If you’re facing a situation that requires prompt attention, we encourage you to visit SilverLake ER. Our team is equipped to provide emergency stitches and comprehensive consultations to address your specific needs. Go to SilverLake ER for timely and expert care, or check in with us today.